Views: 0 Author: Site Editor Publish Time: 2026-01-28 Origin: Site











A sore knee or shoulder can feel like a mystery. You hear “scope surgery” and wonder if it’s a quick fix or a big deal. That’s where arthroscopic surgery comes in.
In this article, we explain what arthroscopic surgery is, how doctors do it, and what problems it can treat. You’ll also learn key benefits, real risks, and what recovery usually looks like, so you can make smarter decisions before any procedure.
Arthroscopic surgery, also called arthroscopy, is a minimally invasive joint procedure. A surgeon inserts a small camera into the joint. They watch the joint on a screen and use slim tools to treat problems.
It can be used to diagnose pain and swelling. It can also treat tears, loose tissue, or damaged cartilage. Many cases are outpatient, so you often go home the same day.
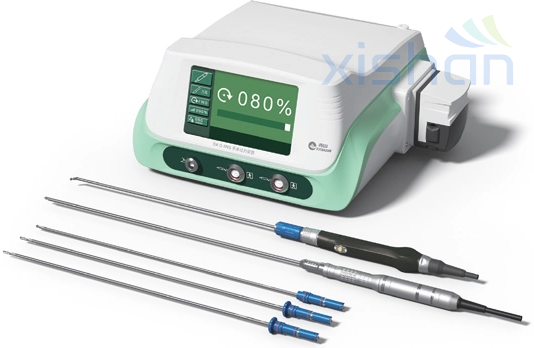
The arthroscope is a thin tube that holds a camera and a light. It sends real-time images to a monitor. That view helps the surgeon see tissue detail inside a tight space.
The joint is usually filled with sterile fluid during the case. The fluid opens the space and clears blood. That makes the picture sharper and helps tool movement.
Some arthroscopic surgery is mainly diagnostic. It confirms what imaging suggests, and it checks cartilage and ligaments directly. This can help when symptoms do not match an MRI report.
Many cases are both diagnostic and therapeutic. The surgeon looks around first, then treats what they find. They might trim a torn edge, repair a tear, or remove loose fragments.
Most arthroscopic surgery happens in big, active joints. Knee and shoulder scopes are common because sports injuries often hit them. Hip arthroscopy is also growing, often for impingement or labral issues.
Smaller joints can be scoped too, such as the ankle, wrist, or elbow. The goal is the same: see inside, then treat through small portals.
Joint | Common arthroscopic surgery goals | Typical situations |
Knee | Meniscus work, cartilage smoothing, loose body removal | Sports twists, catching or locking, swelling |
Shoulder | Labrum repair, rotator cuff work, decompression | Instability, tendon tears, impingement signs |
Hip | Labrum repair, femoroacetabular impingement shaping | Groin pain, deep pinching pain, limited rotation |
Ankle | Debridement, cartilage work, bone spur cleanup | Persistent pain after sprain, stiffness |
Wrist / Elbow | Loose tissue removal, cartilage checks, ligament care | Chronic pain, mechanical symptoms |
Arthroscopic surgery often targets soft-tissue tears. In the knee, this may include a meniscus tear. In the shoulder, it may include a labrum tear or rotator cuff tear.
It can also handle cartilage issues, like rough edges that cause catching. It may remove “loose bodies,” which are small floating fragments. In some cases, it supports ligament work, like parts of ACL reconstruction.
Arthroscopic surgery fits people who have a clear structural problem. It also fits people who tried rest, therapy, or injections, and still struggle. The best candidates have symptoms that match the diagnosis.
Some people should pause and ask more questions first. Severe arthritis often responds less to “cleanup” scopes. Active infection, poor skin health, or unstable medical issues also raise risk. A good surgeon will explain what it can fix, and what it cannot.
Note: Arthroscopic surgery is not always “minor,” even if cuts are small.
Most plans start in the clinic, not the operating room. The surgeon reviews your story, exam findings, and imaging. They also check your goals, like returning to sport or reducing daily pain.
You may need labs or a pre-op visit for anesthesia clearance. You will also get instructions about eating, drinking, and medicines. If you take blood thinners, they will guide timing changes.
In arthroscopic surgery, the surgeon makes a few small incisions called portals. They insert the scope through one portal and instruments through others. They view the joint on a monitor and move tools under camera guidance.
They may shave frayed tissue, anchor a tendon, or repair a labrum. They may also smooth cartilage or remove fragments. The team keeps the joint irrigated so the view stays clear.
Tip: For B2B teams, consistent instrument sets reduce delays and tray errors.
At the end, the surgeon removes tools and drains fluid. They close small incisions using sutures, strips, or glue. They place a dressing, and sometimes a brace or sling.
Recovery begins right away in the post-op area. Nurses monitor pain, nausea, and vital signs. Many people go home the same day, but someone must drive them.
Arthroscopic surgery uses smaller incisions and less tissue disruption. That often means less early pain and less blood loss. It also tends to leave smaller scars.
It can also improve visualization inside some joints. The camera can zoom into corners that are hard to see in open views. That can help precision in the right cases.
Open surgery can be better when tissue damage is extensive. It can also help when the surgeon needs broad access or strong reconstruction. Some fractures, complex revisions, or severe deformities may need open work.
Your surgeon may also choose open surgery if arthroscopy would take too long. Longer time can raise swelling and clot risk. The best approach is the one that fits the problem.
People often assume arthroscopic surgery always heals faster. Sometimes it does, but the diagnosis drives the timeline. A rotator cuff repair is still a tendon repair, even if it is arthroscopic.
Ask what tissue is being repaired and how it must be protected. That answer explains your rehab plan better than the incision size. It also helps you plan work, driving, and sports.
Factor | Arthroscopic surgery | Open surgery |
Incisions | Small portals | Larger cut |
Soft-tissue disruption | Often lower | Often higher |
Early pain and swelling | Often less, not always | Often more |
Best fit | Targeted repairs, joint inspection | Complex reconstructions, broad access needs |
Recovery driver | Diagnosis and repair protection | Diagnosis and repair protection |
A big benefit of arthroscopic surgery is reduced trauma to skin and muscle. That can make early rehab easier, especially for motion work. It may also lower infection risk compared to large open cuts.
It also supports faster return to light daily activity for many cases. People often shower sooner and move sooner. Still, “faster” depends on what was repaired.
Arthroscopic surgery is great for mechanical problems. It is less reliable for pain that comes from advanced arthritis. If the joint surface is worn down, trimming tissue may not change the main pain driver.
Some “cleanup” procedures also have mixed results in some groups. Your surgeon should explain expected benefit in plain terms. If the goal is unclear, it is okay to seek a second opinion.
Every surgery has risk, and arthroscopic surgery is no exception. Infection is uncommon, but it can happen. Blood clots are rare, but risk rises in long cases or high-risk patients.
Nerve irritation can occur from portal placement or swelling. Stiffness can happen if swelling stays high or rehab starts late. Pain flare-ups can also happen if you do too much too soon.
Note: If pain, fever, or redness rises fast, call your surgeon.
The first week is about calming the joint. Expect swelling, soreness, and limited motion. Ice, elevation, and simple exercises help reduce stiffness.
Keep dressings clean and follow shower rules from your clinic. Watch for drainage, heat, or odor. If you have a sling or brace, use it as directed.
Rehab usually moves through phases. Early on, the goal is safe motion and swelling control. Later, the goal is strength and control around the joint.
In repair cases, protection comes first. Therapists may guide passive motion before active lifting. Your plan should match what tissue was repaired.
Phase | Time range (typical) | Main goals | Common limits |
Early recovery | Week 0–2 | Control pain, reduce swelling, protect repair | Brace or sling, no heavy lifting |
Motion phase | Weeks 2–6 | Restore range safely, improve daily function | Slow progression if repaired tissue |
Strength phase | Weeks 6–12 | Build strength, improve endurance, better mechanics | Avoid high loads early |
Return phase | 3–6+ months | Sport or job demands, impact tolerance | Depends on diagnosis (needs verification) |
Timelines vary because jobs vary. Desk work may return sooner if pain is controlled. Physical work may need weeks or months, especially after repairs.
Driving depends on alertness, safe steering control, and medication status. If you use opioids or a sling, do not drive. Sports return depends on strength and confidence, not only time.
Tip: Employers can reduce downtime by offering light duty and remote options early.
Call if fever develops or incisions look infected. Call if calf pain or shortness of breath appears, since clots can be serious. Also call if numbness worsens or the hand changes color.
Some swelling is normal, and some bruising is expected. But severe pain that keeps rising is not typical. If something feels “off,” trust that signal and ask.
Cost is not one number in most systems. It includes surgeon fees, facility fees, anesthesia, and supplies. Repairs that use anchors or implants often cost more.
Rehab is also part of the total cost. Physical therapy visits add up, and missed therapy can extend recovery. Ask for an estimate that includes surgery and rehab planning.
Ask what diagnosis they are treating and what the goal is. Ask what they will do if they find more damage than expected. Ask what restrictions you will have, and for how long.
You can also ask about pain control plans and the need for therapy. Ask about common complications for your exact procedure. A good team will answer clearly and calmly.
Experience matters most for your specific joint and procedure. Ask how often they do your type of arthroscopic surgery. Ask what outcomes they track, like return to sport or revision rates.
Support matters too. Strong clinics coordinate PT, provide clear home exercise plans, and respond fast to concerns. These systems reduce confusion and help recovery stay on track.
Arthroscopic surgery is a minimally invasive way to look inside a joint and treat real mechanical problems. It uses a small camera, tiny incisions, and specialized tools to repair tears, remove loose tissue, and improve function. It often supports faster early recovery than open surgery, but results still depend on the diagnosis and the rehab plan. Knowing the steps, benefits, limits, and risks helps you set realistic goals and avoid common mistakes.
For hospitals and surgical centers, consistent equipment performance also matters for safe, efficient arthroscopy workflows. Chongqing Xishan Science & Technology Co., Ltd. supports arthroscopic surgery teams with dependable medical power solutions designed for stable output, smooth handling, and reliable service. That kind of support helps reduce downtime, improve OR efficiency, and keep procedures running on schedule.
A: Arthroscopic surgery is a joint procedure using a small camera and tiny incisions to diagnose or fix damage inside the joint.
A: Arthroscopic surgery uses small portals and less tissue disruption, while open surgery uses a larger incision for wider access.
A: Arthroscopic surgery can treat mechanical issues like tears or loose bodies, and it often allows earlier motion and smaller scars.
A: Arthroscopic surgery cost depends on the facility, anesthesia, implants, and rehab, so the final price varies by procedure and location.
A: After arthroscopic surgery, call your surgeon if pain rises fast, redness spreads, fever appears, or your calf hurts or swells.
 +86-23-65764808
+86-23-65764808